

Knowing if chemotherapy follows Mohs surgery depends on cancer spread; learn more.
You won't usually need chemotherapy after Mohs surgery. It's often sufficient for treating skin cancers. However, rarely, if the cancer has spread or is very aggressive, you might need other treatments, like chemotherapy.
Mohs surgery demonstrates high effectiveness in treating various skin cancers, including basal cell carcinoma, squamous cell carcinoma, and melanoma. You experience high cure rates for primary basal cell carcinoma, with a 99% five-year survival rate, far exceeding the 90% rate for standard excision. Recurrence rates are also significantly lower: 99% vs. 90% for primary BCC.
For recurrent BCC, you achieve a notable 94% five-year cure rate, surpassing standard excision (94% vs 83%). This exceptional outcome highlights Mohs surgery's advantages in preserving healthy tissue to the maximal extent.
Comprehensive margin analysis is a key Mohs advantage. It ensures you receive a near-complete removal of cancer cells for primary and recurrent disease, reducing the risk of future recurrences.
In squamous cell carcinoma, you see impressive outcomes with primary cSCC. Your five-year cure rate is a robust 97%, better than standard excision's 92%. High-risk cSCC cases also benefit, demonstrating a 95.7% five-year disease-specific survival rate. This reflects the surgical precision and comprehensive margin analysis of Mohs surgery.
You'll also experience reduced local recurrence and metastasis (96.9% five-year local recurrence-free survival and 93.8% regional metastasis-free). Long-term survival benefits are also substantial, with a mean survival time of 18.6 years for high-risk cSCC patients.
For melanoma, your local control rates are extremely high (99.86% for invasive melanoma). Recurrences are also rare (0.14% true local scar recurrences). Your disease-specific survival is likely superior compared to historical wide local excision data.
Moreover, the Mohs advantage of using immunohistochemistry enhances accuracy. You can have a multidisciplinary approach employed in advanced melanoma cases. These Mohs advantages provide effective and precise surgical treatment options.
Given the high cure rates and low recurrence risks associated with Mohs surgery, chemotherapy is typically unnecessary. Mohs surgery's microscopic approach ensures all cancerous cells are removed during the procedure, minimizing the need for further treatments. This powerful surgical technique often eliminates the need for systemic therapies.
Your surgical recovery is prioritized, and your specific case dictates post-surgical care decisions. Comprehensive patient education about the procedure and its outcomes is critical. Chemotherapy is avoided if your skin cancer is effectively treated with Mohs surgery.
Here's why you mightn't need chemotherapy after Mohs surgery:
Your post-Mohs recovery focus is on surgical healing, not systemic treatments. This surgical method offers minimal scarring and a favorable cosmetic outcome.
Detailed patient education regarding your specific case and the nature of skin cancer is essential for complete understanding. The effectiveness of Mohs surgery for localized, treatable skin cancers often renders chemotherapy unnecessary.
Cancer can be categorized as either local or systemic, impacting treatment approaches. Local cancer remains confined to its original site, while systemic cancer has spread to other parts of the body.
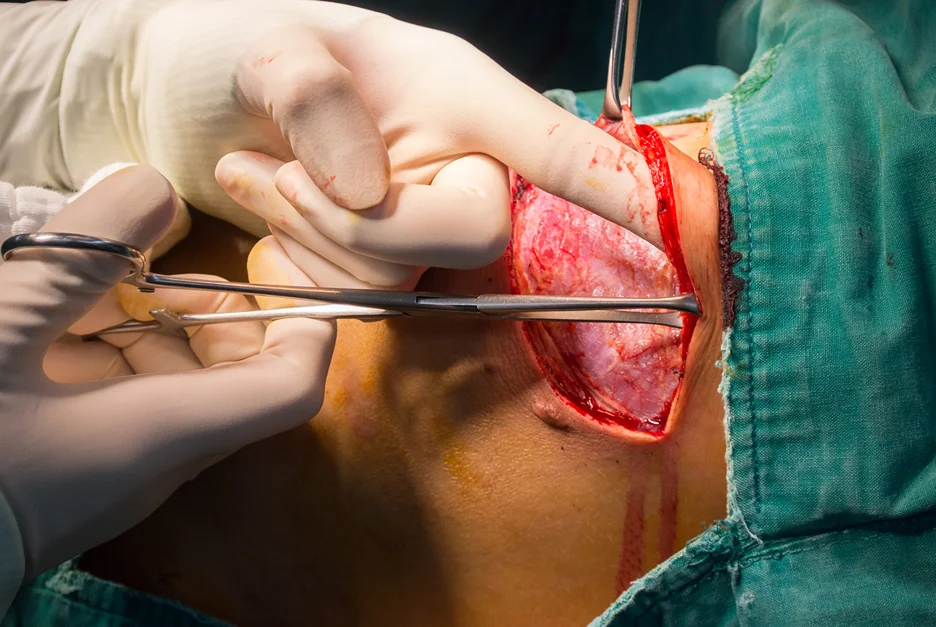
You're diagnosed with local cancer if the disease hasn't spread and is contained within a specific area, like the skin. This often means Mohs surgery is an effective treatment option, removing the cancerous cells while preserving healthy tissue, aiming for high cure rates. For instance, Mohs surgery is often a first-line approach for skin conditions like basal cell carcinoma and squamous cell carcinoma. The surgeon meticulously removes layers, examines them under a microscope, and assures complete tumor eradication.
Systemic cancer, however, implies the cancer has metastasized, traveling beyond the initial site via the blood or lymphatic system, seeding secondary tumors elsewhere. This necessitates systemic treatments, including chemotherapy, a crucial part of your strategy as it targets cancer cells throughout your body.
Simply put, chemotherapy combats systemic cancer by circulating medications to affected areas. A crucial point is that Mohs surgery alone isn't sufficient to treat systemic cancer. Treatment in these cases often involves a multi-pronged approach with chemotherapy employed alongside other methods, like radiation therapy or immunotherapy for the most effective outcome.
You should understand that chemotherapy isn't always required, depending on the stage and type of local cancer.
While Mohs surgery is often curative for local skin cancers like basal cell carcinoma and squamous cell carcinoma, there are rare instances where chemotherapy might be considered. This rare chemotherapy is typically reserved for specific, complex scenarios. You might need it if your cancer has metastasized to other parts of the body, a very rare event following typical Mohs surgery for BCCs and SCCs.
Here are 3 situations in which this might occur:
Large tumors, deep invasiveness, or incomplete removal during surgery might necessitate a complex discussion about additional treatments.
However, alternative local treatments like radiation or further surgery are generally more common than starting chemotherapy.
Remember, chemotherapy is a systemic therapy, used to target cancer cells throughout the body. This is different from surgery and radiation, which only target the site of the cancer.

Perhaps surprisingly, several factors influence whether Mohs surgery is the best approach for your skin cancer. Location matters greatly. Sensitive areas like the head and neck, eyelids, or genitals, demand precise tissue preservation to maintain function and appearance.
Tumor size and depth are crucial. Large tumors, those extending below the subcutaneous fat, or tumors with unclear edges require Mohs for comprehensive removal. Tumor type and recurrence history greatly affect treatment decisions. Recurrent BCCs or SCCs, particularly those in scar tissue, may benefit from the precise surgical approach of Mohs.
Patients with poor outcomes from standard excisions or those with aggressive pathologies may also be surgical candidates. Overall, your health and immunity also play a role. Patients with suppressed immunity, or those needing minimal tissue loss to avoid future procedures, might benefit from Mohs.
These complex factors, combined with specific characteristics of your cancer and individual health, impact treatment timelines and surgical decision-making for surgical candidates. Factors such as the specific characteristics of the tumor, your overall health, and the location of the cancer influence the necessity of Mohs surgery in cases that require a deeper understanding to determine if standard treatments will suffice.
Importantly, post-Mohs surgery monitoring is crucial for optimal healing and long-term prevention of recurrence. You'll need to follow-up diligently to ensure proper wound care and early detection of any issues. Suture removal typically occurs within 2-4 weeks, followed by further evaluations to monitor wound healing. Additional skin checks happen regularly, at 3 and 6 months post-surgery, before you're discharged to a general dermatologist. Adhering to these appointments is essential.
Successfully managing skin cancer necessitates ongoing vigilance. Regular skin checks are vital for early detection of new or recurring skin cancers since you have a nearly 50% chance of developing another skin cancer in the next 2-3 years. You need to learn to recognize skin cancer symptoms and promptly report any unusual developments to your doctor.
While recurrence at the same site is rare due to high Mohs success rates, monitoring remains essential. You'll discuss sun exposure guidance and the treatment of pre-cancerous lesions.
Here's a summary of key post-operative expectations:
Early detection minimizes the risk of recurrence and improves outcomes. Your long-term follow-up appointments may continue for several years. Your commitment to regular skin checks and adherence to your doctor's instructions are crucial for long-term recovery and the detection of new or recurring skin cancers.
Several alternative treatment options exist for skin cancer besides Mohs surgery, each with its own pros and cons. You have choices beyond Mohs, including superficial radiation therapy (SRT), non-Mohs surgical excision, curettage and electrodessication, and superficial radiotherapy with SRT-100™. Understanding these options helps in informed decision-making.
| Treatment Option | Advantages | Disadvantages |
| SRT | SRT advantages include minimal cosmetic impact, suitable for patients unsuitable for surgery. | Higher recurrence risk, especially with ill-defined tumors. |
| Non-Mohs Options | These Non Mohs options offer less specialized equipment and training needs, potentially combining with other techniques. | Increased scarring and larger wounds possible. Less precision in removing only cancerous tissue. |
| Curettage & Electrodessi | Efficient for specific, superficial cancers. Less invasive. | Higher risk of recurrence in certain cases. Possible scarring and pigmentary changes. |
| SRT-100™ | High cure and non-recurrence rates, doctor's office procedure, minimal scarring, no downtime. | May not always be the best option for all skin cancers. |
Choosing the right alternative treatment depends on individual factors, including lesion characteristics, patient health, and personal preferences. Your doctor can provide personalized recommendations based on your specific situation, considering the individual benefits and limitations of each. Weighing the SRT advantages alongside other Non Mohs options is vital to make an informed decision.
Recurrence after Mohs surgery is a possibility, influenced by various factors. Incomplete excision, aggressive tumor biology, and field cancerization can all contribute. Immunosuppression and the surgeon's skill also play a role. Monitoring strategies and recurrence patterns are crucial for early detection.
Here are key factors to consider:
Recurrence often presents within two years as small lesions. Regular self-skin exams and dermatologist check-ups (every 1-3 months to 6 months) are essential monitoring strategies. Early detection is key for the best outcomes.
Dermatologic imaging plays a role in identifying potential recurrence. BCC recurrence rates are generally low, while SCCs and Merkel cell carcinomas have higher rates. Melanoma recurrence depends on the tumor's aggressiveness.
Patients with conditions like CLL may experience higher recurrence rates for BCC. Open communication with your doctor helps understand your individual risk and necessary monitoring strategies.

Knowing the potential for recurrence after Mohs surgery, understanding your treatment options is vital. Patient education and treatment awareness are crucial for informed decisions.
For basal cell carcinoma (BCC), chemotherapy is rarely used, as it's typically localized and Mohs surgery often achieves high cure rates. If the BCC is advanced or metastatic, targeted therapies, like vismodegib or sonidegib, are preferred options over chemotherapy.
Alternative treatments like radiation therapy might be considered for specific situations, such as areas challenging to operate on. Topical therapies, like 5-fluorouracil, are sometimes used depending on the BCC's stage.
For squamous cell carcinoma (SCC), chemotherapy's role is more significant. It might be used when the cancer has spread or conventional approaches aren't viable.
Chemotherapy drugs like cisplatin and 5-fluorouracil may be part of the treatment plan for advanced SCC. Again, chemotherapy isn't a first-line approach, but may be considered for situations when surgery and radiation aren't suitable options.
The choice of treatment, including any alternative therapies, will depend on the specific type and stage of your cancer, as well as your overall health.
These decisions will be made with patient input and thorough consideration of potential side effects. Your doctor should provide detailed patient education about all possible treatments, their implications, and your unique circumstances.
If your desired appointment type or preferred provider is unavailable online, kindly call (978) 525-0100 for Peabody, MA and (603) 742-5556 for all New Hampshire locations. Alternatively please feel free to send us your request via the patient portal, or via email at info@dermskinhealth.com
*For medical dermatology appointments in MA please dial (978) 525-0100 or fill out the appointment request form above.