


If you have basal cell carcinoma (BCC), Mohs surgery is often the preferred treatment, especially for tumors in sensitive areas like the face or those with aggressive histologic subtypes.
This method is ideal for larger, deeply invasive, or recurrent BCCs, as well as for patients with suppressed immune systems. Mohs surgery offers high cure rates of up to 99% for new cases and 94% for recurrent cases, thanks to its precise microscopic examination of 100% of the tumor margins. It minimizes scarring and preserves healthy tissue, making it a gold standard for treating BCC in critical areas.
When considering treatment for basal cell carcinoma (BCC), Mohs surgery is often the preferred method due to its high efficacy and tissue-conserving nature.
Here are the key indications for why Mohs surgery might be the best choice for you:
Mohs surgery is particularly suitable for BCCs located in sensitive or cosmetically sensitive areas, such as the central face, eyelids, nose, lips, chin, ears, and genitalia. These areas are classified under the "H" zone, where tissue conservation is crucial to maintain both functional and aesthetic outcomes.
Your doctor may recommend Mohs surgery if your BCC has aggressive histologic subtypes, such as morpheaform, infiltrating, or micronodular, or if there's perineural involvement.
If your BCC has recurred after previous treatment or if you have a suppressed immune system due to conditions like organ transplants or lymphoma, Mohs surgery is often the preferred option.
Patient education is essential in understanding the benefits of Mohs surgery over other surgical alternatives.
Unlike traditional surgical methods, Mohs surgery allows for the examination of 100% of the tumor margins, ensuring a higher cure rate and minimizing the risk of recurrence.
This precision makes Mohs surgery the gold standard for treating high-risk BCCs.

The precision and efficacy of Mohs surgery make it a beacon of hope for patients battling basal cell carcinoma (BCC), offering several compelling benefits that set it apart from other treatment methods.
One of the most significant advantages of Mohs surgery is its exceptionally high cure rate. For basal cell carcinoma, the cure rate is up to 99% for new cases and up to 94% for recurrent cases, making it the most effective treatment available.
Here are some key benefits of Mohs surgery:
| Benefit | Description |
| Highest Cure Rate | Up to 99% for new BCC cases and up to 94% for recurrent cases |
| Minimal Scarring | Preserves healthy skin by using the smallest incision possible |
| Low-Cost | Performed in an office setting, reducing hospital costs |
| Local Anesthesia | Safer and more comfortable compared to general anesthesia |
| Precise Tissue Examination | Examines 100% of the surgical margins microscopically to ensure complete removal |
These advantages make Mohs surgery an attractive option for patient education, highlighting it as a superior surgical alternative. The procedure's ability to maximize healthy tissue preservation and its low risk of recurrence are crucial factors that patients should consider when evaluating surgical alternatives.
Incorporating Mohs surgery into your treatment plan can provide peace of mind and optimal outcomes, making it an invaluable choice for managing basal cell carcinoma.
In determining the suitability of Mohs surgery for basal cell carcinoma, the characteristics of the tumor itself play a crucial role. One of the key factors is the tumor size. Larger tumors, especially those exceeding 1 cm in diameter, often require more precise and thorough removal methods, such as Mohs surgery, to ensure complete excision and minimize the risk of recurrence.
For instance, nodular basal cell carcinomas that have grown beyond 1 cm can develop central ulcers surrounded by rolled edges, a characteristic known as a "rodent ulcer," which may necessitate Mohs surgery due to their potential for deep invasion.
Another critical characteristic is the tumor depth. Basal cell carcinomas that grow deeply into the skin can wrap around nerves and blood vessels, and even invade muscles and bone if left untreated.
Mohs surgery is particularly beneficial in these cases because it allows for the precise examination of the tumor margins during the procedure, ensuring that all cancerous cells are removed while preserving as much healthy tissue as possible. This is especially important for aggressive subtypes like morpheaform or sclerosing basal cell carcinomas, which often have poorly defined margins and a higher risk of local recurrence.
Patients with certain factors are at higher risk and may particularly benefit from Mohs surgery for basal cell carcinoma. One of the primary risk factors is age; as you get older, your cumulative sun exposure increases, raising your likelihood of developing basal cell carcinoma (BCC). Most BCCs appear in people over the age of 50, and the risk continues to rise with age due to the buildup of sun damage over time.
Your immune status is another critical factor. If you have a weakened immune system, whether due to conditions like HIV, lymphoma, or leukemia, or from treatments such as chemotherapy or immunosuppressive drugs for organ transplants, you're at a higher risk for developing BCC. This compromised immune state makes it harder for your body to repair damage from UV exposure, increasing your cancer risk.
Other high-risk factors include a history of skin cancer, such as previous BCC, squamous cell carcinoma, or melanoma, and exposure to UV radiation from both the sun and indoor tanning.
Individuals with light skin, particularly those with blond or red hair and light-colored eyes, are also more susceptible. Additionally, men are more likely to develop BCC than women, partly due to greater sun exposure.
Understanding these risk factors can help you and your healthcare provider decide if Mohs surgery, with its high cure rate and minimal tissue damage, is the best treatment option for your basal cell carcinoma.
When basal cell carcinoma (BCC) occurs in sensitive anatomic locations, Mohs surgery often emerges as the most effective and conservative treatment option. These locations, particularly on the face, ears, and neck, pose unique challenges due to their complex facial anatomy and the need for precise cosmetic outcomes.
Mohs surgery is highly valued in these sensitive areas because it offers surgical precision that minimizes tissue loss and preserves the natural appearance of the face. During the procedure, the surgeon removes the tumor layer by layer, examining each layer under a microscope until no cancer cells remain. This technique ensures that only the necessary amount of tissue is removed, reducing the risk of disfigurement and promoting better healing.
In areas like the nose, lips, or around the eyes, where tissue sparing is crucial, Mohs surgery provides the best chance of complete tumor removal while maintaining the functional and aesthetic integrity of the area.
The precision and thoroughness of Mohs surgery make it an ideal choice for treating BCC in sensitive anatomic locations, where both cancer treatment and cosmetic results are paramount. This approach helps you achieve a high success rate in cancer removal and an optimal recovery outcome.
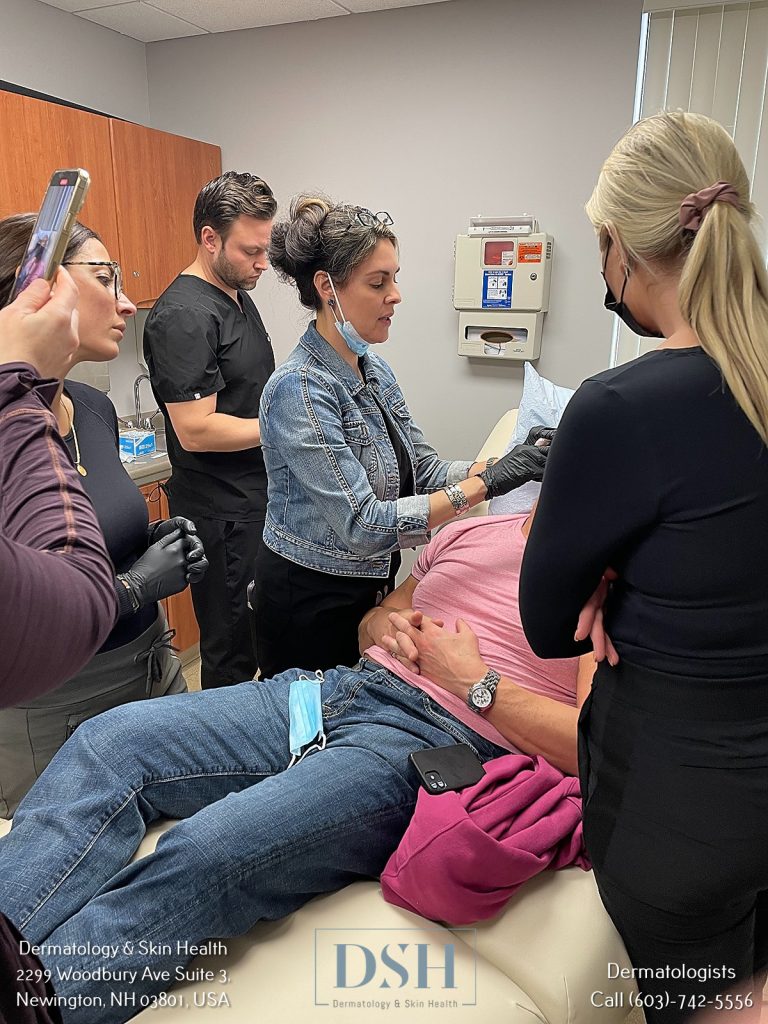
The Mohs surgery process begins with the preparation of the surgical site, where a local anesthetic is administered to numb the area completely. This ensures you remain comfortable and awake throughout the procedure.
The surgeon then removes the visible portion of the tumor using careful surgical techniques, often with a scalpel or a curette to define the clinical margin between tumor cells and healthy tissue.
The next step involves mapping the tumor. The removed tissue is divided into sections, color-coded with dyes, and a detailed map of the surgical site is drawn. This map serves as a guide to track exactly where each small portion of tissue originated.
In the laboratory, the tissue sections are frozen, sliced into very thin sections, and placed on microscope slides. The Mohs surgeon then examines these slides under a microscope to search for any remaining cancer cells at the edges and undersurface of the tissue.
If cancer cells are found, the process is repeated, with the surgeon removing additional layers of tissue only from the precise areas where cancer cells remain. This Mohs technique ensures surgical precision, spares healthy tissue, and minimizes the scar size.
The process continues until all tissue margins are clear of cancer cells, at which point the surgeon discusses reconstruction options and post-operative care.
This meticulous approach is what makes Mohs surgery so effective, with cure rates exceeding 99% for new cancers and 95% for recurrent cancers.
During the microscopic examination phase of Mohs surgery, the surgeon's attention shifts to the laboratory where the removed tissue is meticulously processed and analyzed. This critical step involves several precise microscopic techniques to ensure the complete removal of the basal cell carcinoma.
The tissue specimen is first frozen and then sectioned into thin layers using a cryostat microtome. These layers are then stained with hematoxylin and eosin (H&E) or, in some cases, with immunohistochemical (IHC) staining for more complex tumors like melanoma. The stained sections are placed on slides and examined under a microscope by the Mohs surgeon.
The histological analysis is thorough, with the surgeon examining 100% of the peripheral and deep margins of the tissue specimen. This is achieved by sectioning the tissue in a horizontal direction, which allows for a comprehensive evaluation of the tumor margins, unlike traditional vertical sectioning methods that examine only a small portion of the margins.
If any cancer cells are detected at the margins, the process is repeated, with additional layers of tissue removed and analyzed until the margins are clear of tumor cells. This meticulous approach ensures that all cancerous tissue is removed while conserving as much healthy tissue as possible.
Following the successful removal of the basal cell carcinoma through Mohs surgery, your focus shifts to the critical phase of post-procedure care and recovery. This period is crucial for ensuring proper wound healing and managing any discomfort.
Immediately after the surgery, you'll have a bandage on the wound, which should remain in place for 24 to 48 hours. Your doctor will provide specific instructions on wound care, but generally, you'll need to keep the area clean and dry. You may use mild soap and water or 3% hydrogen peroxide to cleanse the wound, followed by applying petroleum jelly and covering it with a non-stick dressing.
Pain management is also a key aspect of your recovery. Most patients experience mild to moderate pain, which can be managed with over-the-counter medications like acetaminophen or ibuprofen. Applying cold compresses to the area can also help reduce swelling and alleviate pain.
You will need to avoid strenuous activities for 7-21 days and avoid bending or heavy lifting for at least 48 hours. Stitches, if used, will typically be removed after 7-14 days.
Protecting the area from sun exposure with sunscreen (at least SPF 30) is essential to prevent further damage and aid in the healing process.
Mohs surgery boasts some of the highest cure rates among skin cancer treatments, making it a highly effective option for basal cell carcinoma. For new cases of basal cell carcinoma, Mohs surgery has a cure rate of up to 99%, while for recurrent cases, the cure rate is up to 94%.
This high success rate is attributed to the precise layer-by-layer removal and microscopic examination of the tumor and its margins. Unlike other treatment options such as excisional surgery or cryotherapy, Mohs surgery ensures that 100% of the margins are checked, significantly reducing recurrence rates.
When comparing treatment options, Mohs surgery stands out due to its ability to spare healthy tissue while completely removing the cancer. This approach minimizes scarring and cosmetic impact, making it particularly advantageous for tumors located in sensitive areas like the face, eyes, or ears.
If your desired appointment type or preferred provider is unavailable online, kindly call (978) 525-0100 for Peabody, MA and (603) 742-5556 for all New Hampshire locations. Alternatively please feel free to send us your request via the patient portal, or via email at info@dermskinhealth.com
*For medical dermatology appointments in MA please dial (978) 525-0100 or fill out the appointment request form above.