

Lower eyelid reconstruction after Mohs surgery for eyelid skin cancers can be a complex task due to the delicate nature of the eyelid tissues and complex eyelid anatomy. Thorough surgical planning and selection of the proper reconstructive surgery technique are paramount to achieving an optimal functional and cosmetic outcome.
This article aims to provide an overview of lower eyelid reconstruction after Mohs surgery, focusing on surgical planning, technique selection, and postoperative management.
Mohs micrographic surgery is a specialized technique for skin cancer removal while minimizing damage to surrounding tissues. Mohs surgery involves precisely mapping and sequentially removing cancerous tissue in microscopic layers until no more tumor remains. This allows for the highest cure rate with the least amount of normal tissue loss.
Indications for Mohs surgery of the eyelid include basal cell carcinoma, certain squamous cell carcinoma, and sebaceous cell carcinoma.
Lower eyelid reconstruction is necessary after Mohs surgery when defects involve critical structures such as the eyelid margin, canaliculi, or tarsus. The goals of lower eyelid reconstruction include:
An aesthetic outcome that minimizes distortion and synergizes with the patient's facial anatomy is also crucial to achieve an optimal result.
A thorough review of eyelid anatomy is crucial for appropriately planning lower eyelid reconstruction. The lower eyelid is composed of the anterior lamella (skin and orbicularis muscle) and the posterior lamella (tarsus, conjunctiva, and canaliculi). The tarsal plate provides structural support and shape while the canaliculi facilitate tear drainage.
Blood supply to the eyelid comes from the angular, lateral palpebral, and inferior palpebral arteries. The medial and lateral canthal tendons anchor the eyelid to the orbital rim.
Careful evaluation of the eyelid defect is performed to assess key factors that will guide reconstruction. Defect characteristics considered include size, shape, depth, involvement of anterior or posterior lamella structures, location relative to the eyelid margin and canthal tendons, and state of the contiguous eyelid tissues.
Lower eyelid defects are typically classified based on the structures involved.
| Defects | Involvement |
| Orbicularis muscle-sparing defects | Mainly the anterior lamella |
| Orbicularis-disrupting defects | Penetrate the muscle |
| Posterior lamellar defects | Loss of the tarsal plate and/or canaliculi |
| Lateral canthal defects | Disruption of the lateral canthal tendon |
| Marginal defects | Loss of eyelid margin tissues |
With a thorough understanding of eyelid anatomy and a comprehensive evaluation of the defect, the oculoplastic surgeon can select the most appropriate reconstructive technique tailored to each individual patient's needs.
Several techniques are available for lower eyelid reconstruction after Mohs surgery, with the choice tailored to the characteristics of the individual defect.
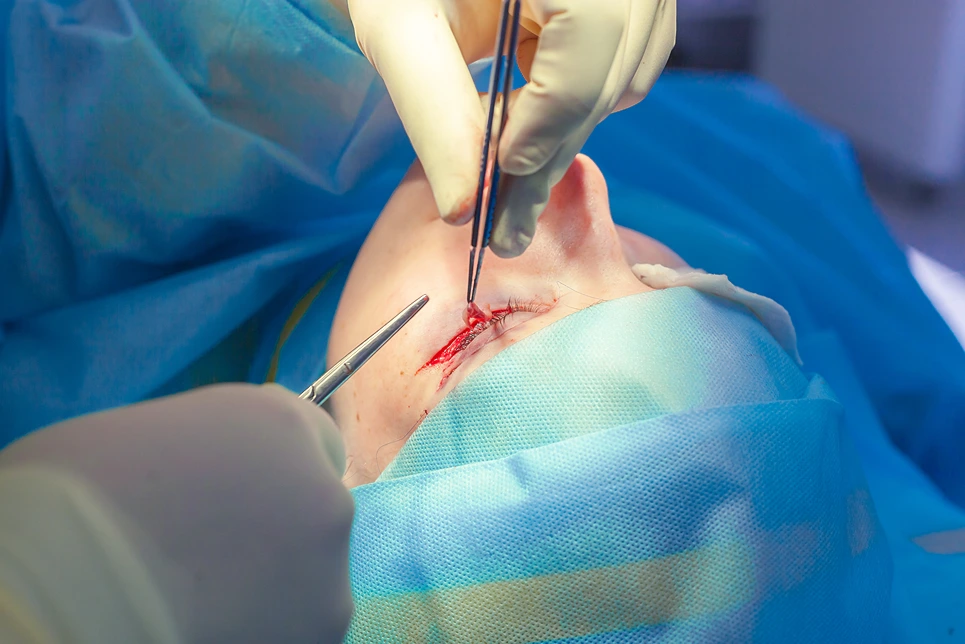
Direct closure is utilized for small, full-thickness surgical defects with adequate laxity of the surrounding eyelid tissues. Closure is performed in a layered fashion, approximating the anterior and posterior lamellae separately. Interrupted or vertical mattress sutures are typically used. Direct closure aims to disrupt the delicate eyelid anatomy as little as possible.
Skin grafts are an option for defects with minimal orbicularis muscle disruption and adequate posterior lamellar support. Full-thickness or thin split-thickness grafts can be used to resurface the anterior lamella while preserving eyelid function. Postoperative monitoring for contraction and elevation is important.
Skin flaps are workhorse techniques for larger defects or those involving the posterior lamella or extensive orbicularis muscle loss. There are various types of skin flaps:
| Technique | Description |
| Advancement flaps | Utilize adjacent eyelid or periorbital skin to advance into the defect. |
| Rotation flaps | Rotate a tubed flap on a vascular pedicle into the defect. |
| Cutler-Beard flap | Uses upper eyelid skin to close lower eyelid defects. |
| Median forehead flap | Provides a concealed donor site and thin, pliable skin for reconstruction. |
| Myocutaneous Flaps | Skin and orbicularis muscle flap with a good match for color, texture, and function. |
| Tarsoconjunctival Flap | Pedicled flap from upper eyelid conjunctiva and tarsus to reconstruct lower eyelid. |
| Rhomboid Flap | Designed in a rhomboid shape for defects near the medial canthus. |
| Conjunctival Flap | Based on conjunctiva for small lower eyelid defects, useful at the medial canthus. |
Several important measures are implemented in the immediate postoperative period to optimize outcomes following lower eyelid reconstruction.
For the first few days, an eye pad and dressing are typically applied to protect the operated eyelid. Antibiotic ointment is frequently prescribed to reduce the risk of infection. Oral antibiotics may also be given. Steroid drops or ointment can minimize inflammation. Analgesics are used to manage postoperative pain.
Careful monitoring in the first few weeks after surgery is important to detect potential complications. Edema, hematoma, wound dehiscence, and infection can be identified on early follow-up visits. Signs of flap vascular compromise like excessive pallor, delayed capillary refill or necrosis require prompt intervention. Contracture and elevation of skin grafts are monitored. Lagophthalmos and eyelid malposition may also develop.
Regular follow-up examinations, usually at 1 week, 2 to 3 weeks, and 6 to 8 weeks after surgery, allow the surgeon to assess the progress of wound healing and the status of flap vascularity, eyelid alignment, contour, function, and cosmesis. Any necessary adjustments, revisions, or additional procedures can be identified and addressed.
With appropriate dressings, medications, close monitoring, and timely follow-up examinations in the postoperative period, minor complications can often be managed conservatively while more serious issues are identified early to optimize functional and aesthetic outcomes of lower eyelid reconstruction.
While most lower eyelid reconstruction cases follow a similar approach, some situations present unique challenges that require additional consideration.
Recurrent tumors after Mohs surgery can result in larger defects involving more extensive tissue loss. This may require complex flap reconstruction, staged procedures, or the use of tissue expanders to achieve adequate closure. Scar tissue from previous surgeries can make dissection and flap harvest more difficult.
Patients with a history of previous eyelid surgery often have scarring, inadequate eyelid laxity, and deformities that complicate reconstruction. Preexisting conditions like eyelid retraction, entropion, or ectropion must be addressed. Reconstruction may require multiple procedures to optimize functional and cosmetic outcomes.
Larger or more complex defects pose significant challenges, especially those involving structural loss or disruption of multiple eyelid lamellae. Combined anterior and posterior lamellar defects often necessitate complex reconstruction with myocutaneous flaps, palatal grafts, or acellular dermis. These techniques require advanced surgical expertise and carry a higher risk of complications.
In these difficult situations, a multidisciplinary team approach involving an oculoplastic surgeon with specialized expertise in complex eyelid reconstruction may be needed. Advanced techniques, staged procedures, and tissue expansion can be considered to achieve the best possible functional and aesthetic outcomes even in the most challenging cases of lower eyelid reconstruction.
Lower eyelid reconstruction after Mohs surgery for eyelid skin cancers requires the expertise of subspecialty-trained ophthalmic plastic surgeons and dermatologic surgeons. Achieving optimal functional and aesthetic outcomes that restore patients' quality of life depends on thorough surgical planning, selection of the most appropriate reconstructive techniques, and meticulous postoperative management.
If you or a loved one is experiencing eyelid defects, dysfunction, or deformities due to eyelid skin cancers or previous eyelid surgery, it is important to consult with experts who have extensive training and experience in eyelid reconstruction.

The doctors at Dermatology and Skin Health offer comprehensive care for eyelid skin cancers and all aspects of eyelid reconstruction. Our team is specially trained in Mohs micrographic surgery.
Whether you need a routine eyelid cancer removal, consultation on the best reconstructive option for your eyelid defect, or complex multi-stage eyelid reconstruction, the expert doctors at Dermatology and Skin Health can help you achieve the best functional and cosmetic outcomes.
If you have questions about lower eyelid reconstruction after Mohs surgery, eyelid malignancies, or eyelid deformities, contact Dermatology and Skin Health today. Our specialists are here to guide you through your eyelid concerns and restore your vision and self-confidence.
If your desired appointment type or preferred provider is unavailable online, kindly call (978) 525-0100 for Peabody, MA and (603) 742-5556 for all New Hampshire locations. Alternatively please feel free to send us your request via the patient portal, or via email at info@dermskinhealth.com
*For medical dermatology appointments in MA please dial (978) 525-0100 or fill out the appointment request form above.